Cancer Cell Therapy Program
Part of Stanford Medicine Cancer Center
Leaders in Cancer Cell Therapy
Cell therapy is among the most promising avenues for cancer treatment available today. Stanford researchers helped to develop the first FDA-approved cancer cell therapies, and Stanford remains at the leading edge of CAR T-cell therapy research to expand the use of cell therapy across more types of cancer.
900 Blake Wilbur Drive
Palo Alto,
CA
94304
Phone: 650-723-0822
What We Offer You for Cell Therapy Care
- Pioneering expertise in treating recurrent non-hodgkin lymphoma and recurrent or refractory acute lymphoblastic leukemia Go to Conditions Treated
- Advanced treatment options in cancer cell therapy Go to Treatments
- Team-based approach to treatment planning and delivery to tailor care to your needs Go to Your Care Team
- Clinical trials to harness cell therapy in the fight against additional cancers and noncancerous conditions Go to Clinical Trials
- Comprehensive support services to help you and your family focus on health and healing Go to Support Services
Non-Hodgkin Lymphoma
Non-Hodgkin lymphoma is a cancer. Like other cancers, it starts when cells grow out of control, multiplying and crowding other normal cells.
Non-Hodgkin lymphoma starts in the lymph system, which contains the lymph nodes, spleen, and bone marrow. The lymph system is part of the body’s immune system that protects it from infections and diseases.
Lymph nodes contain the lymph fluid that carries white blood cells through a network of thin tubes spreading through the body.
Acute Lymphoblastic Leukemia
Leukemia is a cancer of the blood. In leukemia, normal blood cells are transformed in ways that lead to high counts of white blood cells called lymphocytes.
Cancer Cell Therapy Guidebook
The Stanford Cancer Cell Therapy care team developed a guidebook to help you understand what to expect before, during, and after cancer cell therapy.
Click here to learn more:
Cancer Cell Therapy Guidebook (PDF) »
Lymphocytes are made by the bone marrow and by organs of the lymph system. The term “acute” means that the disease progresses rapidly.
Acute lymphoblastic leukemia (ALL) is a fast-growing, aggressive cancer. Sometimes ALL also spreads beyond the blood and affects internal organs or other areas of the body.
Treatments
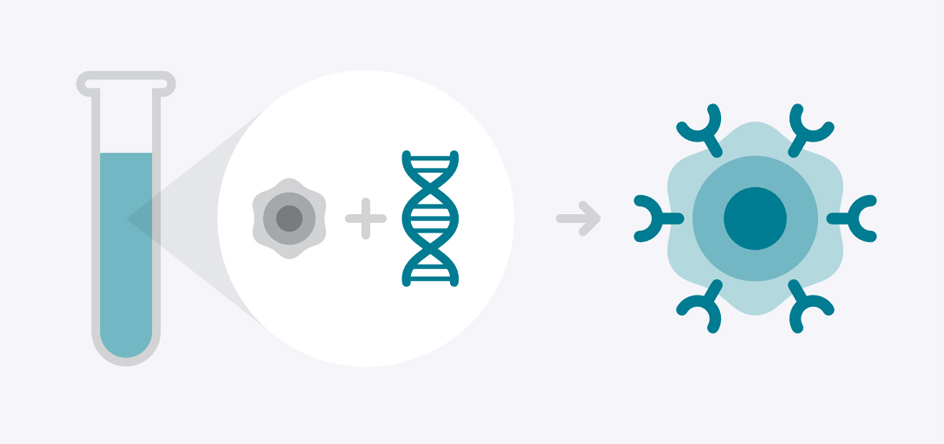
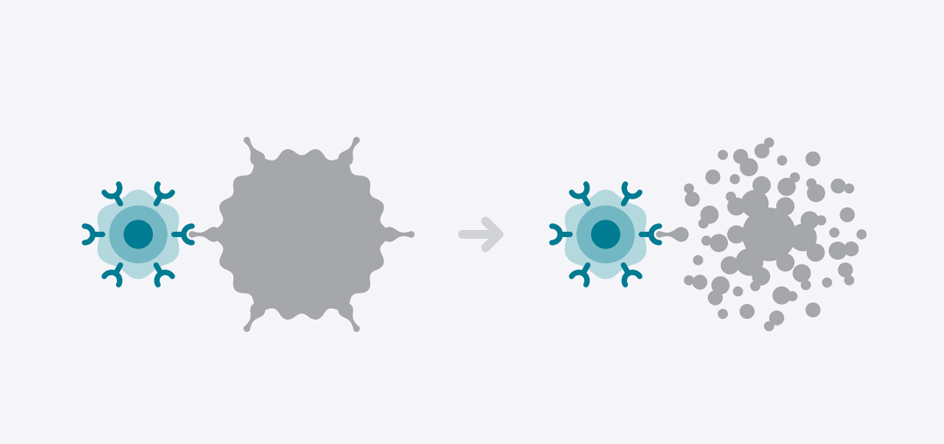
Chimeric Antigen Receptor Therapy, or CAR T-Cell Therapy, is a type of immunotherapy that increases the capacity of immune cells to fight disease. A type of white blood cell called a T-Cell is collected and genetically modified to develop a chimeric antigen receptor. Those receptors attach to cancer cells and kill them.
CAR T-Cell Therapy is approved by the FDA and offered at Stanford for patients with specific types of non-hodgkin lymphoma and acute lymphoblastic leukemia in patients up to the age of 25.
It is available through clinical trials for these diseases and other forms of cancer.
Clinical Trials
We offer one of the nation's most robust Cancer Cell Therapy clinical trial programs. New CAR T-cell treatments are being developed and evaluated at Stanford. As a Stanford Health Care patient, you may be eligible to participate in open clinical trials. Contact your doctor for more information.
Your Cell Therapy Care Team
Each person’s cancer experience is unique, which is why we personalize your treatment plan and care team needs. Our doctors, nurses, technicians, and staff are here to support you. They take part in weekly meetings with colleagues from a number of medical specialties, who will monitor your care and progress.

Your Doctors
Stanford is an Academic Medical Center, which is a type of hospital setting where doctors teach the entire spectrum of medical education. Students range from beginning medical students to fully licensed and practicing doctors completing advanced sub-specialty training. Stanford Medicine is a partnership between Stanford University School of Medicine and Stanford Health Care. Since Stanford is a teaching hospital, you can expect to meet many providers and providers in training.
- Attending Physician: a doctor who supervises doctors in training or in medical school
- Fellow: a doctor doing postgraduate level work and specializing in care of patients with specific conditions
- Resident: a doctor who has graduated from medical school and is in training (also called “residency”) here at Stanford. A resident is also called an intern
- Medical Student: a student who is currently enrolled in medical school with the goal of becoming a doctor

Extended Care Team
This health care provider works with your surgical oncologist to help with diagnosis and treatment. The provider can be a nurse practitioner, physician’s assistant, or clinical nurse specialist.
Nurse coordinators are specialized registered nurses who provide one-on-one support to guide you through the cancer treatment process. The coordinators serve as your point of contact to help manage your care, from your first appointment through follow-up visits. They assess your needs, answer your questions, make referrals, coordinate appointments, and provide patient education.
These assistants help with administrative issues such as scheduling your appointments, managing your paperwork, and requesting your medical records.
If you need to stay in the hospital after surgery, a registered nurse will take care of you.
This team member greets you at the front desk and registers you for your appointments.
When you have apheresis (a specific type of blood transfusion) or chemotherapy, your infusion treatment area (ITA) scheduler will set up your appointments.
This team member helps you during your doctor visits by:
- Bringing you to your exam room after you check in for an appointment
- Providing you with a hospital gown or other clothing for your physical exam
- Taking your vital signs before your doctor sees you
A staff member calls you before your first appointment to:
- Provide information that you need to know to prepare
- Provide a list of what you need to bring
- Help gather your medical records
This health professional works with you and your family to provide emotional support, counseling, and resources such as financial assistance, spiritual counseling, and transportation. A social worker can also connect you with community services and, if you’re coming from out of town, help you find a place to stay.
Stanford has financial specialists to help you understand the many sources of support that are available to you, so you may focus on healing.
This team member tracks the processing, manufacturing and receipt of your personalized cell therapy.
This team member informs you of the opportunity to participate in ongoing clinical trials and clinical outcomes research.

Support Services
Cancer Care Services
Cancer Care Services is your connection to personalized support services before, during, and after your treatment. Our teams of doctors, nurses, social workers, spiritual care providers, nutrition experts, financial counselors, and more work with your oncology team to provide comprehensive specialized care to you and to your family.
- 650-498-6000 Ask for the Cancer Care Services team
Stanford Health Library
For confidential help with your health care questions, contact the Stanford Health Library. Professional medical librarians and trained volunteers can help you access journals, books, e-books, databases, and videos to learn more about medical conditions, treatment options, and related issues.
- 875 Blake Wilbur, Palo Alto: 1st floor near the cafe, 650-736-1960
- South Bay Cancer Center: 3rd floor lobby, 408-353-0197
- Email us your questions: healthlibrary@stanfordhealthcare.org
Our clinic at the Stanford Cancer Center Palo Alto is designed for your convenience. We offer streamlined check-in, same-day appointments to see multiple specialists, and comprehensive medical and support services under one roof. If you're traveling from a long distance to our facilities, our case managers can assist you with travel, housing, and other logistics.
FAQs for Cell Therapy
CAR T-Cell therapy is a type of immunotherapy, which increases the capacity of immune cells to fight disease. A type of white blood cell called a T-Cell is collected and genetically modified to develop a chimeric antigen receptor, or CAR. Those CARs latch onto a specific antigen on the surface of the cancer cell to disrupt and destroy it.
CAR T-Cell therapy is approved by the FDA to treat some forms of non-hodgkin lymphoma and for patients with recurrent or refractory acute lymphoblastic leukemia up to age 25.
There are several ongoing trials of CAR T-cell therapy for other forms of blood cancers and some solid tumors.
We work with patients and insurers to secure health insurance coverage for eligible patients. More insurers are covering care for FDA-approved therapies.
Side effects are generally easier to tolerate than those associated with chemotherapy.
Our care team will monitor your response to the treatment and manage any reactions or complications. Side effects can be mild or more severe but are treatable and generally indicate the therapy has activated the immune system to fight the cancer.
The most common side effect of CAR T-Cell therapy is called cytokine release syndrome or CRS. It can affect up to 9 in 10 CAR T-Cell patients. It is generally brief, lasting about a week. Many patients liken it to the flu with fever, low energy, and body aches. It is treatable with medication.
The other side effect is known CAR T-Cell-related encephalopathy syndrome or CRES. Its symptoms are more severe than those of CRS and may include memory loss or confusion. In rarer cases, they may affect speech. CRES is treatable. Symptoms usually go away after a few days.
Stanford has the knowledge and resources to manage these reactions when then they occur.
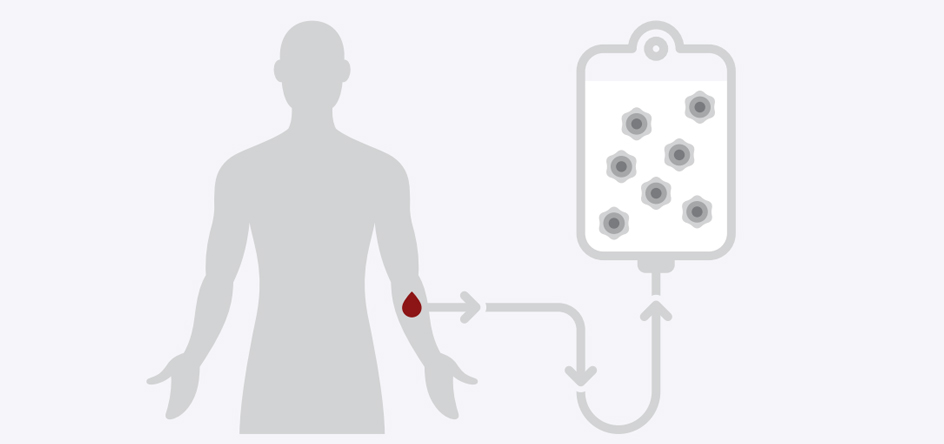
The treatment process involves:
- Evaluation to confirm that CAR T-Cell Therapy is a recommended treatment
- Collection and sorting of blood cells to isolate T-cells for therapy
- Genetic modification of T-cells in a lab to cause them to develop chimeric antigen receptors that target cancer
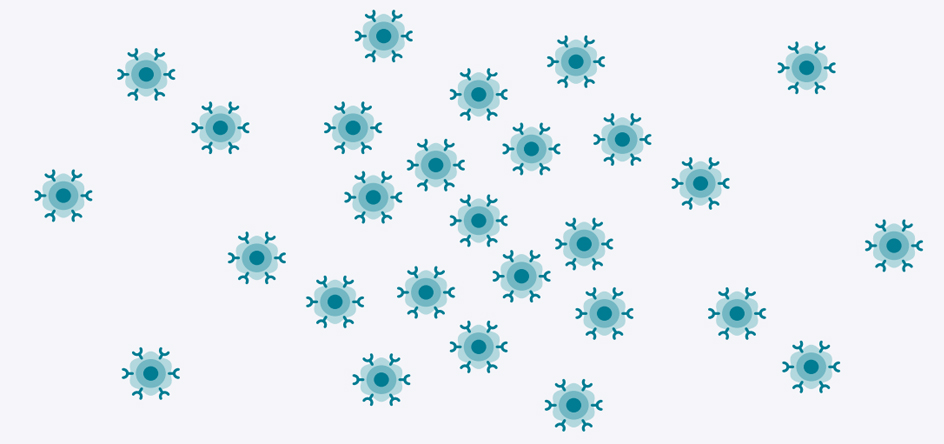
- Culturing these modified cells in a lab to increase the number of available CAR T-cells
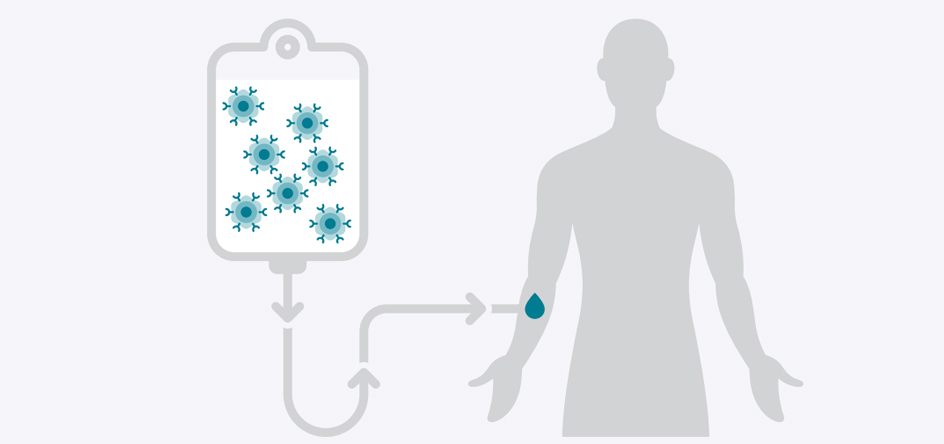
- Preparative regimen of chemotherapy to get your body ready to receive the CAR T-cells
- Infusion of the CAR T-cells into the body
- Recovery of a few months, while your immune system stabilizes and gets stronger
For Referring Physicians
PHYSICIAN HELPLINE
Fax: 650-320-9443
Monday–Friday, 8 a.m.–5 p.m.
Stanford Health Care provides comprehensive services to refer and track patients, as well as the latest information and news for physicians and office staff. For help with all referral needs and questions, visit Referral Information.
You may also submit a web referral or complete a referral form and fax it to 650-320-9443 or email the Referral Center at ReferralCenter@stanfordhealthcare.org.
Are you a patient or physician interested in cancer cell therapy? Call 650-723-0822.