- Specialized expertise at a level 4 epilepsy center with a multispecialty team experienced in advanced diagnostic methods, like inpatient video-EEG (brainwave) monitoring, outpatient EEG monitoring, and computerized brainwave mapping, for epilepsy and conditions imitating epilepsy. Go to Conditions Treated
- Advanced treatment options from an internationally recognized epilepsy center. These include nonsurgical treatments and epilepsy surgery such as neuromodulation to treat complex epilepsy—especially drug-resistant epilepsy. Go to Treatments
- Team-based approach with specialized epilepsy doctors, surgeons, neuroradiologists, neuropsychologists, neuropsychiatrists, and nurses working together. Go to Your Care Team
- Clinical trials that offer access for eligible patients to innovative epilepsy treatments, such as medications, neuromodulation devices, and innovative surgical approaches. Go to Clinical Trials
- Comprehensive support services to help you and your family focus on health and healing. Go to Supportive Services
- Ease of access to comprehensive epilepsy treatment at our Neuroscience Health Center, with options that can help even if previous treatments haven’t. Go to Connecting to Care
Epilepsy and seizures can make your life unpredictable, but the right treatment can help you live a full life. At Stanford Health Care, our multispecialty epilepsy team treats all types of epilepsy, seizures, and conditions imitating seizures, even the most complex cases. Conditions include:
Symptoms of epilepsy include recurring seizures, which are abnormal bursts of electrical activity in the brain. Seizures cause problems with muscle control, movement, sensation, speech, vision, or awareness.
Medications can control seizures in many people with epilepsy. But for up to one-third of people with epilepsy, medications don’t work well, or at all, to control the seizures, or, the medications have debilitating side effects. Intractable, or drug-resistant, epilepsy develops when two anti-seizure medications, taken alone or together, don’t successfully control seizures.
Nonepileptic seizures
Nonepileptic seizures (NES) have symptoms like those of epileptic seizures, but there is no abnormal electrical discharge in the brain. The causes can be psychological (for example, stress accumulated over a lifetime) or physical. Physical causes of NES include fainting, sleep disorders, low blood pressure, complicated migraines, tremors, hypoglycemia, and other medical conditions.
Our Comprehensive Epilepsy Program has received recognition as the highest level (Level 4) epilepsy center from the National Association of Epilepsy Centers.
Our Comprehensive Epilepsy Program is internationally recognized for expertise in epilepsy and seizure disorders. We focus on personalized care to manage symptoms and stop seizures or reduce both their frequency and severity to improve your quality of life.
We partner with you and your family for ongoing care, from evaluation and diagnosis through treatment and follow-up management. Through our Intractable Epilepsy Program, we provide exceptional care for people who have drug-resistant epilepsy.
INNOVATION HIGHLIGHTS
- Stanford Medicine led the development of two FDA-approved devices: Ceribell™, to improve the diagnosis and treatment of people at risk for seizures, and, a dry, wireless EEG.
- Our team collaborates with the Wu Tsai Neurosciences Institute at Stanford University on the latest research innovations in epilepsy treatment.
- We’re internationally recognized for our work in neuromodulation for drug-resistant epilepsy, having led pivotal trials for vagus nerve stimulation, deep brain stimulation, and responsive neurostimulation.
- Stanford Medicine researchers are actively studying how specific brain cells, known as mossy cells, affect the spread of seizures. Stanford Medicine is a world leader in the science of understanding epilepsy.
At Stanford Health Care, our multispecialty team thoroughly evaluates you, taking time to understand your concerns and symptoms. With the latest testing and imaging, we determine an accurate diagnosis to begin planning your treatment.
Our testing for epilepsy includes:
An electroencephalogram (EEG) noninvasive test records your brain’s electrical activity and can help tell us where seizures begin. We can also perform video-EEG monitoring for more details about what you’re experiencing.
Brain imaging can show areas where seizures begin and signs of other conditions that might be causing seizures. Diagnostic imaging for epilepsy can include:
- Computed tomography (CT) scan—uses specialized X-ray equipment to produce cross-sectional images of the brain
- Magnetic resonance imaging (MRI) uses radio waves and powerful magnets to create detailed images that can show brain lesions that may be causing seizures
- High-density EEG—identifies areas in three-dimensional brain space where seizures may begin
- Positron emission tomography (PET) scan—uses an injection of a small amount of a radioactive tracer to picture brain metabolism, which may identify seizure locations
- Single-photon emission computed tomography (SPECT) scan—uses a radioactive substance to show blood flow in the brain during seizures
Neuropsychological testing is a series of tests that assess a wide range of cognitive (thinking) and behavioral functions. Neuropsychological tests evaluate memory, attention, concentration, language, problem-solving, and other abilities, often identifying dysfunction of particular regions of the brain.
Neurosurgeons place electrodes in or on your brain to record electrical activity more precisely. Functional mapping helps us plan surgery by showing where seizures begin and identifies areas of critical brain function, such as language, sensation, and movement. This is needed only for a subgroup of epilepsy surgery candidates.
In preparation for surgery, a Wada test locates the areas in your brain that control speech and memory. This test helps us plan a surgical approach that effectively treats seizures while preserving healthy brain tissue.
If you have drug-resistant epilepsy or recurring seizures, we conduct in-depth testing and 24/7 monitoring in our epilepsy monitoring unit. You may stay in the EMU for several days as our team tracks your symptoms to plan more effective treatment.
Nonsurgical Therapies
Many people with epilepsy and seizures find relief with anti-seizure medications and other nonsurgical treatments.
More than 25 epilepsy medications are available today, and they work in different ways to control seizures. After a thorough evaluation and testing, we discuss options with you for medications that may best treat the seizures you’re experiencing.
You may need to try different medications to find the right one or the right combination. You’ll visit your care team regularly so we can assess your progress and adjust medications as needed. We are also developing artificial intelligence programs to help physicians choose the best drug for you.
Depending on the symptoms and type of seizures you’re experiencing, nonsurgical therapies may be right for you. Options include:
- A ketogenic diet—a strict eating plan with low carbohydrates, moderate proteins, and high fats
- Psychological counseling with our neuropsychologists—helps people with seizures, especially psychogenic nonepileptic seizures, manage emotions and thoughts. Therapies may include cognitive behavioral therapy (CBT) and behavior modification therapy.
If anti-seizure medications haven’t reduced your symptoms or seizures, we may recommend surgery. Epilepsy surgery is a safe, effective option to evaluate and treat seizures. We perform several types of epilepsy surgery, including:
Focal resection is surgery to remove the seizure focus, which may be a brain lesion, or part, or all, of a brain lobe. We perform this surgery for people who have seizures in only one area of the brain that can be safely removed.
The corpus callosum is a band of nerve fibers connecting the two halves (hemispheres) of the brain. It helps the hemispheres share information, but it also contributes to the spread of seizure impulses. This operation separates the corpus callosum to stop seizures from spreading between hemispheres.
This surgery removes part of the temporal lobe, an area of the brain near the temples and ears. Temporal lobectomy is the most common type of epilepsy surgery.
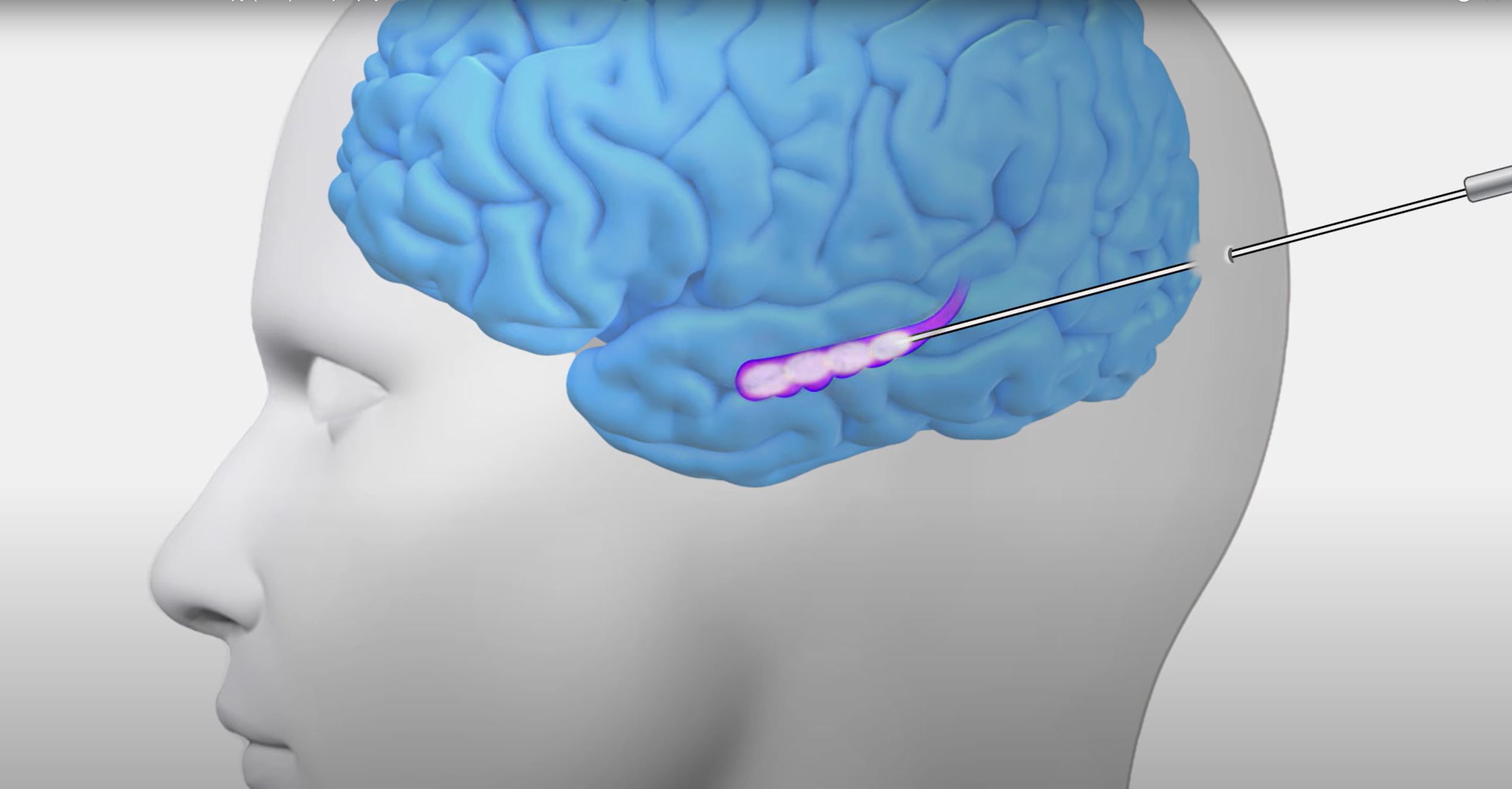
Neurosurgeons perform a minimally invasive procedure to access a seizure focus through a small opening in the skull. A laser wire is guided to the seizure focus and heat is applied to destroy the brain tissue.
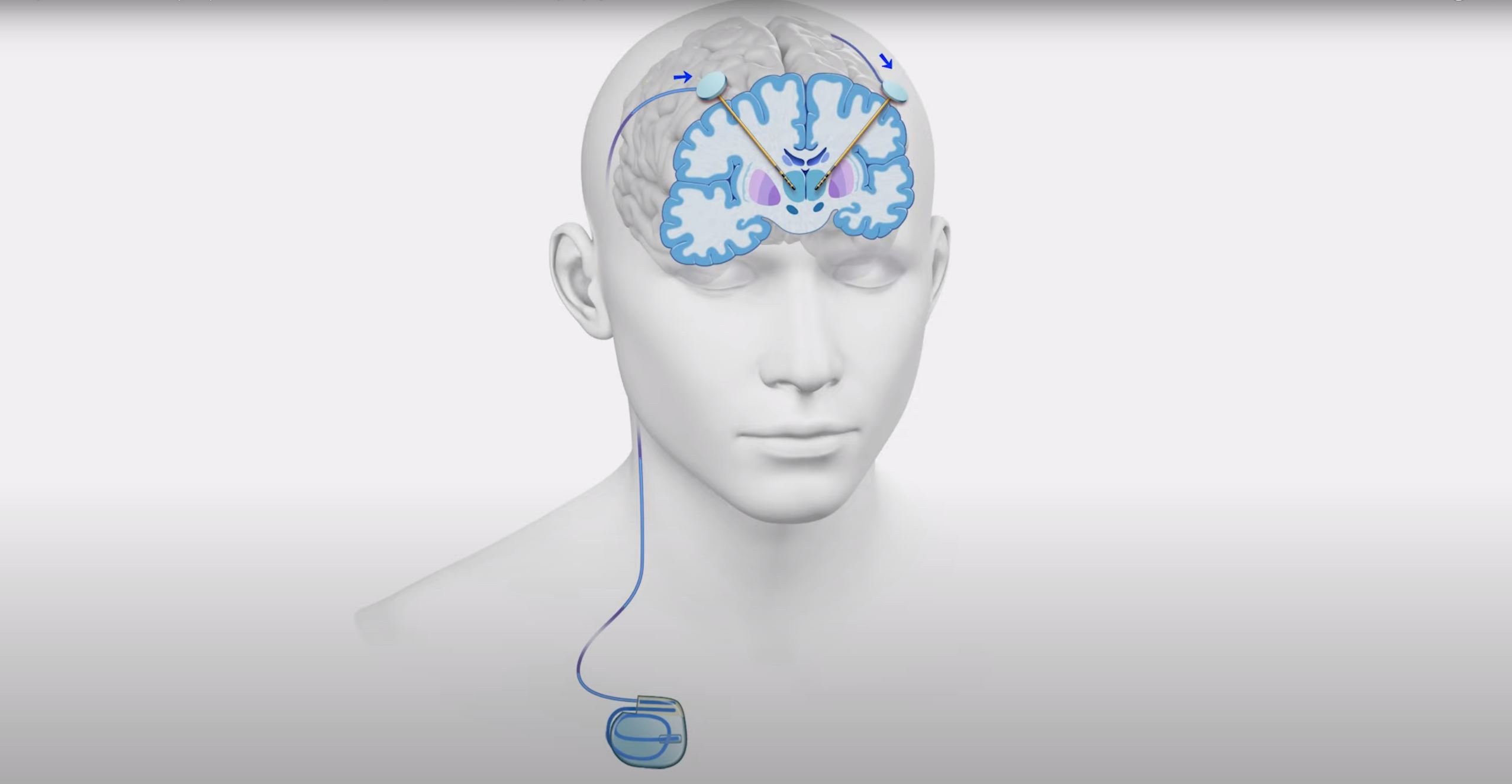
A neuromodulation device, sometimes called a neurostimulation device, is a treatment option for people who have drug-resistant epilepsy and are not candidates for epilepsy surgery. Surgeons implant neuromodulation devices in the body or brain, and wires from the devices send mild, painless electrical pulses to control seizures.
Neuromodulation devices are implanted beneath the skin, with no external wires. They are programmed and controlled by external radio paddles. Each neuromodulation therapy works in different ways:
- Deep brain stimulation (DBS) delivers electrical pulses at specific levels and intervals to help prevent seizures or reduce their frequency. DBS is helpful for people who have focal seizures in one or more areas of the brain.
- Responsive neurostimulation (RNS) can help stop seizures before they begin by monitoring brain waves and sending pulses to interrupt unusual electrical activity. RNS can help people who have focal seizures in only one to two well-localized areas of the brain.
- Vagus nerve stimulation (VNS), like DBS, delivers electrical pulses to the neck at regular intervals to treat seizures. With VNS, the pulses travel along the vagus nerve, which runs from the head through the neck into the torso. VNS can treat almost any type of seizure.
Care for neurological disorders goes beyond medical treatments. We encircle you and your family with supportive services to help treat your mind, body, and soul.
Innovation Through Clinical Research
Stanford Health Care Neuroscience actively participates in groundbreaking research and clinical trials to evaluate new and better ways to diagnose, treat, and manage neurological disorders. Participating in a trial may give you access to experimental therapies that are not available otherwise. We also partner with the Wu Tsai Neurosciences Institute to better understand the brain, develop new treatments for brain disorders, and promote brain health.
Clinical Trials
Clinical trials are research studies that evaluate a new medical approach, device, drug, or other treatment. As a Stanford Health Care patient, you may have access to the latest, advanced clinical trials.
Open trials refer to studies currently recruiting participants or that may recruit participants in the near future. Closed trials are not currently enrolling, but similar studies may open in the future.
Your Circle of Care
A diagnosis of a neurological condition—and the changes it may bring—can be unsettling. We offer you and your caregivers the personalized support you need at every step. Your team listens to you and develops a plan for your situation. And you’ll work with the same team from diagnosis throughout treatment, so we can get to know you and your needs.
Each patient's experience is unique, which is why we provide personalized care. Our team tailors treatment and supportive services to meet your individual needs.
Your Doctors
Epileptologist
An epileptologist is a neurologist who specializes in diagnosing epilepsy and seizure disorders and treating them with medications or other nonsurgical options.
View All {0} Epilepsy Specialists »Epilepsy Neurosurgeon
An epilepsy surgeon is a surgeon who specializes in neurology and brain surgery to stop seizures or reduce their frequency. Epilepsy surgeons are an essential part of the care team for people with drug-resistant epilepsy.
View All {0} Epilepsy Neurosurgeons »Advanced Practice Providers (APPs)
Our skilled nurse practitioners specialize in diagnosing and treating spine and brain tumors. They see patients independently and occasionally alongside your doctor. APPs can give you a thorough exam, write prescriptions, and help prevent or treat any issues. Our APPs meet weekly to discuss patient needs.
View All {0} Advanced Practice Provider Doctors »Extended Care Team
Neuropathologist
Neuropathologists specialize in diagnosing conditions of the brain and nervous system through microscopic evaluation of tissue sampled during biopsy or surgery.
View All {0} Neuropathologists »Neuroradiologist
A neuroradiologist is a doctor who specializes in interpreting diagnostic imaging of the brain and nervous system. They work behind the scenes to help provide an accurate image of the brain to show possible structural causes of seizures.
View All {0} Neuroradiologists »Neuropsychiatrist
A neuropsychiatrist is a medical doctor who specializes in neurology and psychiatry to treat mental health symptoms related to neurological conditions. Neuropsychiatrists provide psychosocial counseling and prescribe medications for people with epilepsy who also have mental health symptoms, such as anxiety or depression.
View All {0} Neuropsychiatrists »Epilepsy Nurses
Epilepsy nurses are clinical nurse specialists who have special training in neurology and care management for people with epilepsy. They are experts in patient care, education, and coordination of services for people with epilepsy. They may also participate in research efforts.
Support Services
Your wellness is our top priority. As part of your care, we design a wellness plan to support you and your family before, during, and after treatment.
We offer a wide array of support services to help you to feel your best. Contact our Neuro Care Services for your personal support plan.
We make access to care as simple as possible. We anticipate what you need and provide support when you need it. Our network of locations puts our services within your reach. User-friendly digital health tools help you stay connected with your care team. We accept most insurance plans and offer discounted transportation, short-stay options, and international travel and translation services. We help make sense of the details, so you can make decisions that are right for you.
At the Stanford Health Care Comprehensive Epilepsy Program, we make accessing care easy and convenient. We make every effort to coordinate your appointments so that you can see multiple providers, as needed, during a single visit.
For Referring Physicians
PHYSICIAN HELPLINE
Fax: 650-320-9443
Monday–Friday, 8 a.m.–5 p.m.
Stanford Health Care provides comprehensive services to refer and track patients, as well as the latest information and news for physicians and office staff. For help with all referral needs and questions, visit Referral Information.
You may also submit a web referral or complete a referral form and fax it to 650-320-9443 or email the Referral Center at ReferralCenter@stanfordhealthcare.org.